It was the morning of April 2, 2020 when I gave birth to our third child, Aeda Sicilia IV. We went to the hospital at 3:00 am, excited but at the same time worried of what will happen. Preparations were done upon our arrival but because of Covid-19, additional protocols were done and/or removed.
Upon arrival, we were screened by the receptionist at the OB Complex for possible exposure to people with Covid. We were told to wait for the bedside nurse for further screening. After the second screening, I was told to go inside the complex but husband cannot go inside. I waited inside the labor room along with other mothers who were scheduled for a Caesarean Section Delivery or those who were already in labor.
A fetal monitor was attached to my belly to monitor baby’s heart beat. I was told by the resident OB that I was already experiencing contractions (which I was monitoring for days). Pedia, OB and Anes resident doctors interviewed me and gave me a run through of what will happen. I asked the Anes doctor not to make me sleep during the procedure because I want to experience Unang Yakap. Few hours after, I was hooked to an IV drip and changed my clothes to hospital gown. My BP was checked, thank God it was at 110/70.

Fetal Monitor

Hooked to an IV drip
At 7:00 am, I was rolled in to the delivery room, ready for the procedure as my OB, Dr. Camille Ann Abaya arrived. My OB informed me that husband will not be allowed to be there during the procedure (as they are limiting the number of possible exposure to Covid patients). Nurses prepared the room for the operation and the Anes doctor started to perform spinal anaesthesia.
My OB started the procedure as I can hear her voice. The Anes doctor was by my side all throughout the procedure. She was the one who told me that my OB was about to pull out baby Aeda. When they heard my baby cry, all of them clapped and said their congratulations.

I was put on sleep while they finish the procedure. I was surprised when I woke up that I fell asleep. The Anes doctor said she wanted me to rest instead of just wait for the procedure to finish.
Recovery Room
I was transferred to the recovery room after the procedure with baby Aeda. I was fighting the urge to sleep, probably the effect of anaesthesia that was given to me. Hours passed and we were still at the recovery room. I heard the nurse that the breathing rate of my baby was faster than usual. So they called my husband that it will take few more hours before we will be able to leave the recovery room as they still need to observe the breathing rate of Aeda.
Hours passed, they put Aeda on oxygen support and continued to observe her breathing rate if it will improve. The pedia resident told me that Aeda might be experiencing tachypnea, a condition common to CS delivered babies.
While waiting for their feedback, I was trying to soothe baby by singing songs or humming some hymns. We tried latching her but when the pedia, Dr. Saulog, said that there should be no intake, I just continued to sing and talk to her. One time, I was really sleepy but I needed to hum. I fell asleep while humming and the nurse asked if I was ok. I was humming Ave Maria that time. I was calling all the saints from my childhood to adulthood and prayed to the Infant Jesus of Prague to help Aeda with her breathing. I was already thinking of the worst case that time…that Aeda will not last long (yup, I was that pessimistic that time because I did not know what else to think).
By around 6:00 pm or so, they decided that baby Aeda will be put at the Immediate Care Unit because they oxygen support is not allowed inside the regular room. It broke my heart that I will not be with her during our stay and that I will not be able to breastfeed her.
So they started preparing her and called my husband to go down to the OB Complex so he can see our baby. After they transferred Aeda to the IMCU, I was transferred to my room. My husband was waiting for us at the reception area of the OB Complex.

First night
The first night was very sad for me, with all the hormones and recovery that I was undergoing plus the status of Aeda that time. I talked to my husband about what happened inside the recovery room. The first night, I just slept and rested. I was really tired. From time to time, the nurses will wake me up for my meds and vitals. BP at that time was still at 110/70 and that was something to be thankful for. I was also allowed to eat on full diet but I was not on my right mood to eat thinking that my newborn was alone.
The first morning and the next
The next morning, the nurse from IMCU called my husband and asked if he could go down to see our baby. And so he did.

Aeda at IMCU the morning after. IV at her right foot and oximeter at her left foot.
He was informed that we can go back to her at 1:00 pm so they can give an update from the pedia. As for me, my OB told me that I should pass the gas that day and that I should be able to stand up (but gradually: sit gradually, dangle feet then try to stand up). So while my husband was with Aeda, I lied down on my side (it was very difficult to turn my body because of my incision) to pass the gas. Luckily, it was effective. Thanks to my bedside nurse who told me that trick.
At first, I wanted to try to stand up so I gradually sat down (St. Luke’s beds have the buttons accessible to the patients). But after few minutes, he returned to our room.
After lunch, the nurse at IMCU called my husband and told him that I can start breastfeeding Aeda but I need to go there every 2 hours. So he helped me stand up and it was the most difficult part of this experience. My OB told me that probably it was because I already had 3 CS procedures that’s why it was so painful to stand. It was really painful.
We borrowed a wheel chair from the nurses’ station so I can go to the IMCU and start feeding our baby.

Feeding Aeda at IMCU
I wanted to stay longer but my bedside nurse called and told Aeda’s nurse that I need to go back to the room because of my medicines. I realized that I was also a patient that time, which I forgot because my baby needed me more.
So we go down every 2-3 hours, depending on the nurse on duty. On the second day, April 4, we decided to buy expressed breast milk as top up to my milk so Aeda can recover faster and her bilirubin can be flushed faster. I also experienced plugged ducts because I was not feeding by demand. So I had to visit the lactation unit from time to time to express my milk. On this day, the oxygen support was removed at 6:00 am so Aeda can be weaned from this support. But after lunch, it was returned because her breathing rate started to increase again but it was lowered to 0.25.

Aeda with oxygen support at IMCU
We lack sleep but both of us wanted to see our baby so we really had to get up and go to the IMCU. Besides, Aeda needed to feed.

Aeda with her bilirubin patch
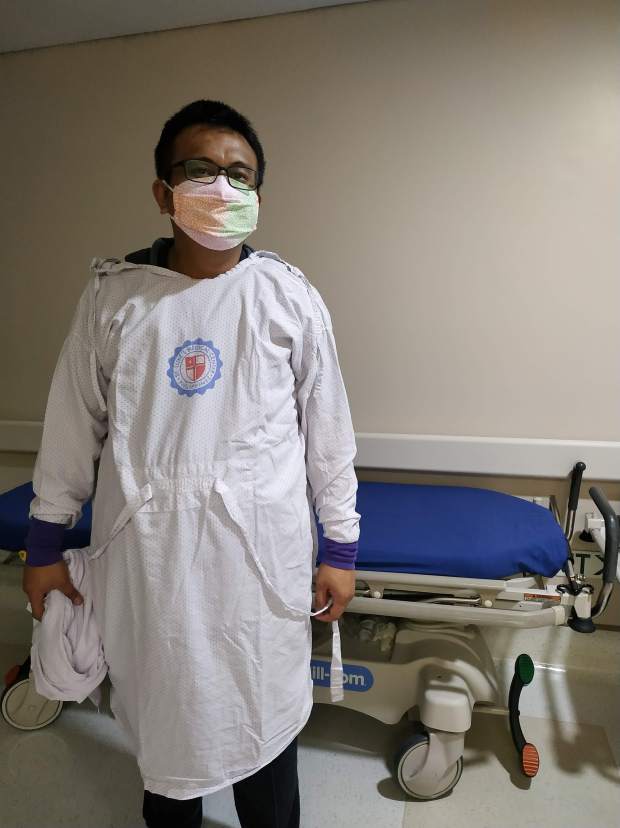
This is how we enter the IMCU every time
The third day
At 4:00 am, her oxygen support was again removed. Bilirubin the previous day was normal. We were waiting for the blood culture before the pedia can decide but we were already informed by the resident doctor that most likely, Aeda will not be discharged.
With a heavy heart, we started to pack our things as I needed to be discharged that day. My discharge order was given at 11:00 am and my bedside nurse already gave me my home care instructions. At 1:00 pm, the IMCU nurse called my husband and told him that Dr. Saulog wanted to see us there for possible discharge. Hopes were high! So we rushed to the IMCU and talked to Aeda’s doctor.
We were informed that everything’s normal including the blood culture (no growth after 2 days and 19 hours). She told us the normal and not normal incidences. Finally, she told us that baby can go home with us. She was also informed by my OB that I was for discharge that day. Probably, that’s the reason why she decided to discharge Aeda too.
It was an answered prayer! For the past days, I asked all those who messaged me to pray for her. I was also praying to the Infant Jesus of Prague every time I have a silent moment. I prayed to St. Josemaria Escriva, Mama Mary and our very own baby Tres to help me pray for Aeda’s good health status and discharge.
It’s time to go home
At past 5:00 pm, we were able to leave the hospital after paying all the bills. I did not ask my husband how much because I just wanted to go home. I just had the idea that the running bill the day before was already at P50,000+ without the professional fee. This was just for Aeda’s stay at the IMCU. My bill was already paid the day before the procedure and it was at P133,000+ (already the package price).
While waiting for the discharge of Aeda, the nurse took my BP. It was already at 120/80. I felt a little worried as I know what was already happening to my body. Same as before, postpartum pre-eclampsia. But I told myself, and I claimed it, that I will not be readmitted like before (during JJ’s time). I continued praying while waiting for my husband. At least we’re going home.
So the kids were surprised when we got home.

The Orzales siblings united at last
Day after discharge and the next: Postpartum Pre-eclampsia episode
I needed to monitor my BP as per my OB. And as expected, it was elevated until I reached 160/100. I already informed my OB and she said if my BP was at constant 140/100 or higher, I need to take my meds.
I was already starting to feel stressed because I do not want to go back to the hospital. The mere thought of magnesium sulfate terrified me. So yes, I was recovering from the operation, taking care of my incision and monitoring my BP at the same time plus hormonal changes, lack of sleep and tired from taking care of a newborn.
Luckily, my husband is also a researcher and searched for vegetables that can lower blood pressure. He made a vegetable shake that I took from time to time while monitoring my BP. Amazingly, my body responded well and my BP started to go down few minutes to one hour after intake. He religiously blended the vegetables and made a shake so I can drink every 2-3 hours.
On April 9, 4 days after discharge, my BP was controlled at 120/80. I also started to wean from the shake. on April 10, I did not drink the shake but my BP was only at 110/80. So I know that I was already out of danger. I was also feeling better. Thank God I did not experience seizure as this could mean I was closer to death by that time. It was another answered prayer and I know that we had a handful of prayer warriors.
Postpartum blues
The hormonal rollercoaster plus my recovery from the operation, financial stress and everything this experience had given us, I am having minor breakdowns. The good thing is that I am aware but even so, I cannot control my emotions. While this is still normal as I am on my second week, I am thinking that prolonged blues can lead to depression…postpartum depression. This is what I want to prevent. I am still struggling at this stage but I am hopeful that this will be another answered prayer.


One thought on “My birthing experience: Aeda”